Yale Researchers Identify New Role for STING in Treatment of Head and Neck Cancer
A recent study conducted by Yale Cancer Center reports the discovery of a new role for STimulator of INterferon Genes (STING) for head and neck cancer treatment. Previously, STING has been related to the immune response involved in DNA damage. However, this study aims to focus on STING’s new role in tumor DNA damage response and the new combinations of therapies this may offer.
The study published in Nature Communications incorporates the use of our Mouse Oral Squamous Cell Carcinoma (OSCC) Cell Line (MOC1). Oral cavity squamous cell carcinoma (OSCC) is a common subset of head and neck cancers and happens to be the 6th most common cancer worldwide. Our Mouse Oral Squamous Cell Carcinoma (OSCC) Cell Lines are available to purchase on our website here.
STING Regulates Cell Death Through Reactive Oxygen Species (ROS) and DNA Damage
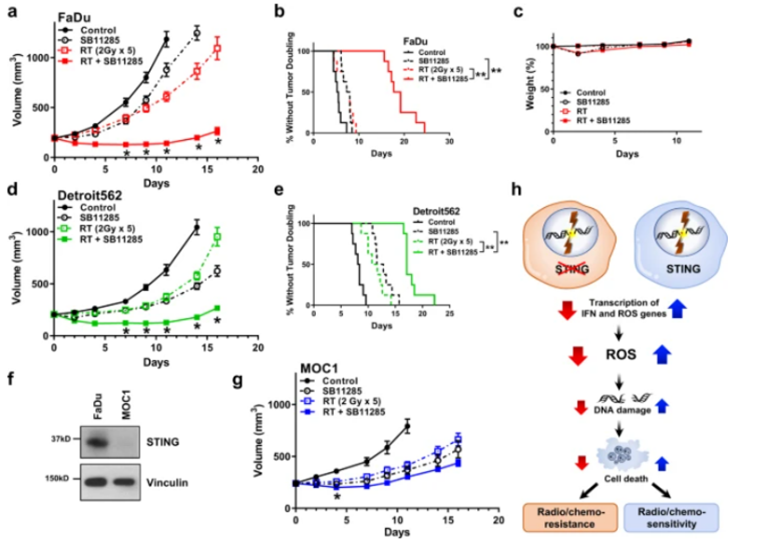
Using a genetic screening-based approach, the Hayman Lab at Yale proposes a new way that STING regulates resistance to DNA-damaging cancer therapies. The study shows how a loss of tumor STING reduces the production of treatment-induced reactive oxygen species (ROS) leading to decreased DNA damage, decreased tumor cell death, and resistance to DNA-damaging therapies.
Thomas Hayman, MD, PhD, Assistant Professor of Therapeutic Radiology at Yale Cancer Center, notes “Excitingly, our results support the clinical evaluation of STING agonists in combination with DNA-damaging treatments in patients with head and neck cancer to improve responses to standard therapies.”
STING Increases the Effectiveness of Cancer Therapies
An analysis of tumor samples from patients with head and neck squamous cell carcinoma validates these findings, suggesting that a loss of STING expression links to worse clinical outcomes. Yale researchers conclude activation of STING with a clinically available STING agonist increases the effectiveness of radiation therapy to decrease head and neck tumor growth.
Scientists suggest a further study using STING as a biomarker for treatment selection is warranted. Joseph Contessa MD, PhD, Professor of Therapeutic Radiology and of Pharmacology and Co-Leader of the Radiobiology and Radiotherapy Research Program at Yale Cancer Center says, “This work shows us an example of the high risk/ high reward screening experiments that will move our field forward to seek better treatments for a wide range of cancers.”
Related Research
Do you work in this field of research? Check out our catalog selection of cancer reagents here, including the Mouse OSCC Cell Line (MOC1) used in this study. View some of our other associated products below:
- MC-38-CEA Cell Lines and MC-38-MUC-1 Cell Line from National Cancer Institute/NIH
- DNA-RNA Hybrid [S9.6] Antibody from National Institute of Allergy and Infectious Diseases/NIH
- Natural Killer Cell [H25] Antibody from Cancer Research Technology
- MUC1 Antibodies from Dana-Farber Cancer Institute
- Macrophage Cell Lines from National Cancer Institute/NIH
- Cancer Angiogenesis and Nanomedicine Services from Tel Aviv University
- KPCY Mouse Pancreatic Cancer Cell Lines from University of Pennsylvania


