New ways to combat antibiotic-resistant pneumonia
Like many other bacterial infections that affect humans, pneumonia has acquired a significant amount of antibiotic resistance, rendering traditional means of treatment ineffective. Researchers have been trying to find new ways to fight pneumonia and other infections for better treatment of patients. Recently, researchers led by Dr. Qingming Hou of Boston Children’s Hospital and Dr. Fei Liu of the Chinese Academy of Medical Sciences/Peking Union Medical College published a study in the Journal Science Translational Medicine where they mobilized neutrophils to fight bacterial pneumonia.
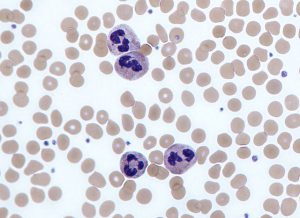
Purple-stained neutrophils surrounded by platelets and red blood cells. Credit: Graham Beards.
Neutrophils
Neutrophils are a type of white blood cell mobilized to the site of infection when an immune response is triggered. Neutrophils seek out and kill bacteria (and other pathogens), but also cause a significant amount of inflammatory substances to be released. The resulting inflammation can impart significant damage on the lungs’ air sacs. Although the bacterial infection may be eliminated, lasting damage to the lung may result.
According to Dr. Hongbo Luo, senior author on the paper, “The question is, when we have pneumonia, do we want to enhance neutrophil function or suppress it? It’s very tricky.”
Continued Research
Dr. Luo’s laboratory at the Boston Children’s Hospital has been studying the enzyme IP6K for years. They found that in neutrophils, IP6K inhibits signaling of another molecule, PIP3. The result of inhibiting IP6K was that there were increased levels of PIP3 in neutrophils, which activated the neutrophils and kept them living longer. They killed more bacteria and Luo said they acted “like ‘super’ neutrophils.”
A Surprise
Dr. Lou’s group, with the collaborators at the Chinese Academy of Medical Sciences and Peking Union Medical College, worked with a mouse model of bacterial pneumonia. When they deleted the IP6K1 gene in these mice, neutrophils were much more active – engulfing and killing more bacteria. The real surprise, however, was that fewer neutrophils gathered in the lungs, reducing damage.
“The exciting thing is that bacterial killing is high, and tissue damage is low,” said Dr. Luo in a press release. Additionally, rather than genetically knocking out the IP6K1 gene in the mouse model, the investigators used TNP, a drug known to inhibit IP6K, to treat the mice, and the results were similar.
What is the Mechanism?
The researchers next wanted to determine why less neutrophils accumulated in the lungs without IP6K activity. The key was platelets, whose function is to stop bleeding by clumping and clotting at the site of infection or injury. Platelets produce polyphosphate which affects neutrophils. Dr. Luo explained, “When we inhibit IP6K, platelets make less polyphosphate, reducing neutrophil recruitment.”
A Wide-reaching Treatment
As neutrophils are involved in non-specific combat of invaders to the body – whether it be bacteria, viruses or tumor cells, the results of this study may have implications that reach beyond pneumonia. Reduction of neutrophil recruitment via IP6K inhibition may be effective in the treatment of other infections and cancer.
Do you study bacteria or other infectious disease? Kerafast offers a wide range of antibodies and other reagents to fuel your research. Materials related to this area of research include:
- Neutrophil specific, NIR fluorescent imaging agent from University of Virginia
- Human neutrophil CAP-18 antibody from Montana State University
- Platelet factor antibodies from Blood Center of Wisconsin
- Metapneumovirus glycoprotein antibody from Icahn School of Medicine at Mount Sinai
- Polyphosphates from University of Michigan


