What’s a Patient-Derived Xenograft?
Here at Kerafast, we recently added the first patient-derived xenograft model to our online platform. Developed at Virginia Commonwealth University, this xenograft was derived from a 74-year-old female patient with non-small cell lung cancer (NSCLC) and fully characterized in an Oncotarget journal article. The xenograft’s addition to our catalog prompted us to ask the question: what exactly is a patient-derived xenograft?
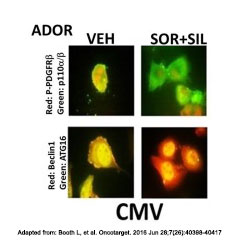
The NSCLC Patient Derived Xenograft (ADOR) was recently added to the Kerafast platform by the lab of Paul Dent, PhD, Virginia Commonwealth University.
Patient-derived xenograft (PDX) models, as it turns out, are created when a human tumor is implanted directly into an immunodeficient mouse. These models offer a new and increasingly popular approach for preclinical in vivo testing of anti-cancer compounds.
Drug discovery and development researchers have a great need for realistic models that can accurately predict how humans will respond to a given therapeutic. Drugs often seem promising in preclinical studies, only to fail in human clinical trials. In fact, it has been said that only 5% of anti-cancer compounds with preclinical promise actually make it to market. These failures are costly and take limited resources away other research.
Part of the problem is that traditional cancer models – such as established cell lines or xenograft models derived from those cell lines – do not accurately represent primary human tumors. Patient-derived xenograft models help address that issue, preserving the structural and genetic features of an original patient tumor. For example, PDX models retain the cellular heterogeneity, tumor vasculature, stromal reaction and gene expression profiles of human carcinomas.
In addition, studies have suggested that the response of PDX models to potential cancer drugs correlates well with human clinical response. Studies have been conducted across various types of cancer, including breast cancer, colorectal cancer and ovarian cancer. PDX models therefore provide a useful tool for evaluating and predicting the efficacy of anti-cancer compounds.
PDX models have also shown promise in personalized cancer treatment. In this scenario, researchers create mice “avatars” from a patient’s tumor. They can then test various drugs, in various combinations, trying to find the treatment that would work best for that specific patient. One research paper, for example, identified the most efficient chemotherapy combination for a woman with metastatic breast cancer. The personalized medicine applications of PDX models have also been covered by mainstream media; check out an article on the topic from The New York Times.
Despite their promise, PDX models still face various challenges and limitations. First, the engraftment and expansion process can take months and is not always effective. Then, once the model is created, it is expensive to house the mice. Traditional PDX models also do not allow for studies of immunotherapy treatments, a hot area in cancer research, because the mice do not have an immune system. In addition, the models are not ideal for research into metastasis or the effect of tumor microenvironment.
Despite these drawbacks, PDX models offer an exciting tool for in vivo preclinical testing of cancer drugs. To learn more about the topic, here are two recent review articles we recommend:
- Pompili L, et al. Patient-derived xenografts: a relevant preclinical model for drug development. J Exp Clin Cancer Res. 2016 Dec 5;35(1):189.
- Liu ET, et al. Patient-derived tumor xenografts: why now? JAMA Oncol. 2016;2(5):567-568.
Do you work in this area of research? Check out the newly available NSCLC Patient Derived Xenograft, as well as other unique reagents developed by academic investigators for cancer or drug discovery research.


