Cells Ability to Adapt to Hostile Environments in Critically Ill Patients
Researchers at the University of Plymouth collaborated with the University of College London and the Universities of Cambridge and Southampton to demonstrate that cells can adapt to conditions in critically ill patients by producing energy more efficiently than in healthy patients. Their research was published in Redox Biology.
Oxygen and the Electron Transport Chain
Within mitochondria – also known as the powerhouses of our cells—resides the Electron Transport Chain (ETC) where oxygen plays a vital role in cellular respiration (energy production). The ETC is the last step of aerobic respiration and is the only part of glucose metabolism that uses atmospheric oxygen. Protein complexes of the ETC transport electrons facilitated by oxygen inhalation, generate the fuel that drives our cells. Electron acceptors and donors, such as O2 and NADH, move through these complexes to produce energy and yield ATP and water.
Survival from Critical Illness Relates to Changes in Cellular Bioenergetics
“When a body is going through trauma, there’s the temptation to think we need to give more oxygen or stimulate cells to survive,” states lead scientist Dr. Helen McKenna from the University of Plymouth research team. However, the study suggests that some cells can adapt to the conditions they are in and highlights specific modifications that are associated with human resilience during life-threatening stress.
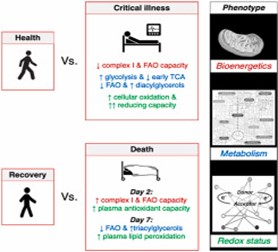
Over the course of seven days, scientists collected muscle and blood samples from 21 critically ill patients (those with two or more organs failing) in intensive care, and 12 healthy people, and compared cell behavior. The team combined their assessment of mitochondrial respiration with metabolomic, lipidomic, and redox profiling to further understand how cells adapt to their environment.
Further, the team measured the capacity of one of the ETC protein complexes, and noticed it was 30 percent lower in survivors than in non-survivors after 48 hours of illness, but tended to increase in seven days, with no such recovery observed in non-survivors. This showed that even though the complex appeared to work at a lower rate, the cells adapted to the adverse conditions of the critical illness. This further supported their hypothesis that critically ill patients produce energy more efficiently than healthy people; thus, demonstrating that cells can adapt to low oxygen levels and still produce the same yield of ATP.
Preparing for Future Studies
The next step is to identify why some people’s cells behave in this way while others don’t. This behavior could be due to genetics, age, or previous exposure to trauma. More research is needed but this work is an important first step to understanding the difference between life or death for critically ill patients. In conclusion, “unravelling the cellular and molecular foundation of human resilience may enable the development of more effective life-support strategies,” says Dr. McKenna.
Related Research
Do you work in this field of research? If so, you may be interested in viewing our other reagents that might be related to cell biology research. Some of the reagents include:


