How Cancer Manipulates the Tumor Microenvironment to Dodge Immune System Attack
A study published in Nature highlights how chemicals in the tumor microenvironment can manipulate the immune system to prevent the immune response that attacks cancer. The research, conducted by a team of scientists at the University of Pittsburgh School of Medicine and UPMC Hillman Cancer Center, suggests an already existing drug could be applied to promote the anti-cancer effects of immunotherapy treatment.
The team, led by University of Pittsburgh professor of immunology Greg Delgoffe, disrupted the tumor microenvironment in mice immune cells. This enabled them to shrink tumors, promote survival and increase immunotherapy sensitivity.
The Kerafast team is pleased to see valuable research advancing the life science industry using reagents available in our catalog. The study cites our MC-38 Cell Line, a murine colon adenocarcinoma cell line frequently used to study cancer, tumors, immunotherapy, T cells, and more. The MC-38 cell line was developed by researchers at the National Cancer Institute and is now available to researchers worldwide via our website here.
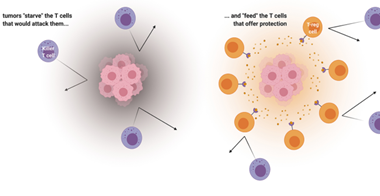
Cancer “feeds” the T cells that protect the tumor and “starves” the T cells that would attack. Credit: UPMC, created with Biorender.com
T Cells and the Tumor Microenvironment
The research team studied the competition to obtain nutrients between tumors and different T cells. They found that killer T cells and regulatory T cells have different appetites, and that cancer takes advantage of this mechanism.
Killer T cells play a large role within the immune system by fighting viruses, bacteria, cancer, and other intruders. Regulatory T cells (T-reg cells) counteract killer T cells, acting as protectors of a body’s own cells and playing a role in preventing the development of autoimmune diseases.
Tumor Cells Recruit T Cells by Providing Food
The team found tumors have larger appetites than T cells, allowing them to eat vital nutrients that killer T cells would typically use to attack. The tumors also excrete lactic acid to feed the regulatory T cells, which turn the lactic acid into energy utilizing a protein called MCT1. This entices T-reg cells to obey the tumor cell to get fed.
As Dr. Delgoffe stated in a press release: “Cancer is wise to the whole situation. Cancer cells don’t just starve T cells that would kill them but actually feed these regulatory T cells that would protect them.”
Silencing MCT1 Protein Promotes Anti-Cancer Effects
In mice with melanoma, researchers found that silencing the gene coding for the MCT1 protein causes tumor growth to slow down and mice to live longer. “We starved the T-regs,” said Dr. Delgoffe. “When T-reg cells are not being sustained by the tumor, killer T cells can come in and kill the cancer.”
The anti-cancer effects were even stronger when Dr. Delgoffe’s team combined MCT1 inhibition with immunotherapy. Potentially, a similar effect may be possible using drugs that inhibit MCT1, one of which is already performing well in clinical trials for people with advanced lymphoma.
Related Research
Do you work in this field of research? Check out our catalog selection of cancer reagents here, including the MC-38 Cell Line used in this study. View some of our other cancer-associated products below:
- MC-38-CEA Cell Lines and MC-38-MUC-1 Cell Line from National Cancer Institute/NIH
- Natural Killer Cell [H25] Antibody from Cancer Research Technology
- MUC1 Antibodies from Dana-Farber Cancer Institute
- Macrophage Cell Lines from National Cancer Institute/NIH
- Cancer Angiogenesis and Nanomedicine Services from Tel Aviv University
- KPCY Mouse Pancreatic Cancer Cell Lines from University of Pennsylvania


