New Findings on the Zika Virus
|
When the Zika virus began making headlines several months ago, scientific knowledge of the virus and its potential impact on humans was relatively slim. Though the virus was discovered in Uganda in the 1940s, Zika did not become a significant research focus until the recent outbreak in Brazil, when the virus became linked to microcephaly in newborn infants. The international scientific community rapidly turned its attention to Zika, and researchers are now working to better understand the virus and its effects, including whether it truly is causing the rise in microcephaly cases. The race is also on to develop medicines and vaccines capable of treating and preventing Zika. Below, we summarize several recent studies to come out of this flurry of research. For more background on the basics of Zika, read our previous blog post, “What is the Zika virus?”. And if you are one of the researchers working to address this outbreak, check out our newly available Zika Virus antibody. Made available by the Dr. James E. Crowe, Jr. lab at Vanderbilt University, the human serum specimen contains polyclonal antibodies induced by natural infection with Zika virus and recognizes the human Zika virus envelope protein (E) gene. First Mouse Model for the Zika Virus Enables Treatment Screening Researchers at the University of Texas Medical Branch, Galveston (UTMB) have developed the first peer-reviewed mouse model for Zika infection reported in decades. The study, published March 28 in the American Journal of Tropical Medicine and Hygiene, paves the way for preclinical testing of potential drug and vaccine candidates. Several candidates have been ready to test, but were held up awaiting availability of a mouse model; the new study removes this hurdle and allows treatment screening to begin. Normal lab mice cannot be infected by the Zika virus, meaning researchers could not determine whether potential therapies treat Zika in mice, a critical first step before a drug candidate is tested in humans. The UTMB researchers tested several genetic varieties of mice to find one affected by the Zika virus and discovered that mice genetically altered to have a deficient innate immune response did develop the disease. In particular, young mice from these strains were highly susceptible to Zika infection. The mouse model is now immediately available for use. “There is a huge demand to screen antivirals that have been backlogged because we haven’t had a good way to test them,” Dr. Shannan Rossi, a UTMB virologist and lead author of the study, explained in a press release. “Without this model, we were really stagnant in our efforts to find new treatments. You can look for efficacy in cell cultures, but that tells you almost nothing about what’s going to happen when you test in a mouse or a human. This will help get those drug and vaccine candidates moving through the pipeline.” |
|
Zika Virus Can Infect Human Neural Stem Cells |
|
| Researchers from Johns Hopkins University and Florida State University have demonstrated that the Zika virus can infect human cortical neural progenitor cells, a type of neural stem cell that generates the brain’s cerebral cortex. This finding is a first step toward understanding how the Zika virus might impact the brains of developing fetuses, though the researchers caution it does not prove a direct correlation between Zika and microcephaly. The results were published in Cell Stem Cell this March.
The research team derived neural cells from induced pluripotent stem cells, and then showed that Zika virus stock grown in mosquito cells could infect those cells. In addition, the infected cells became drivers of Zika virus reproduction; after a single infection, virus particles would spread throughout a stem cell plate within three days. This led to cell death and/or disruption of cell growth. “We are trying to fill the knowledge gap between the infection and potential neurological defects,” said first author Hengli Tang of Florida State University in a press release. “The questions we address here are among the very first questions people want to know the answers of.” |
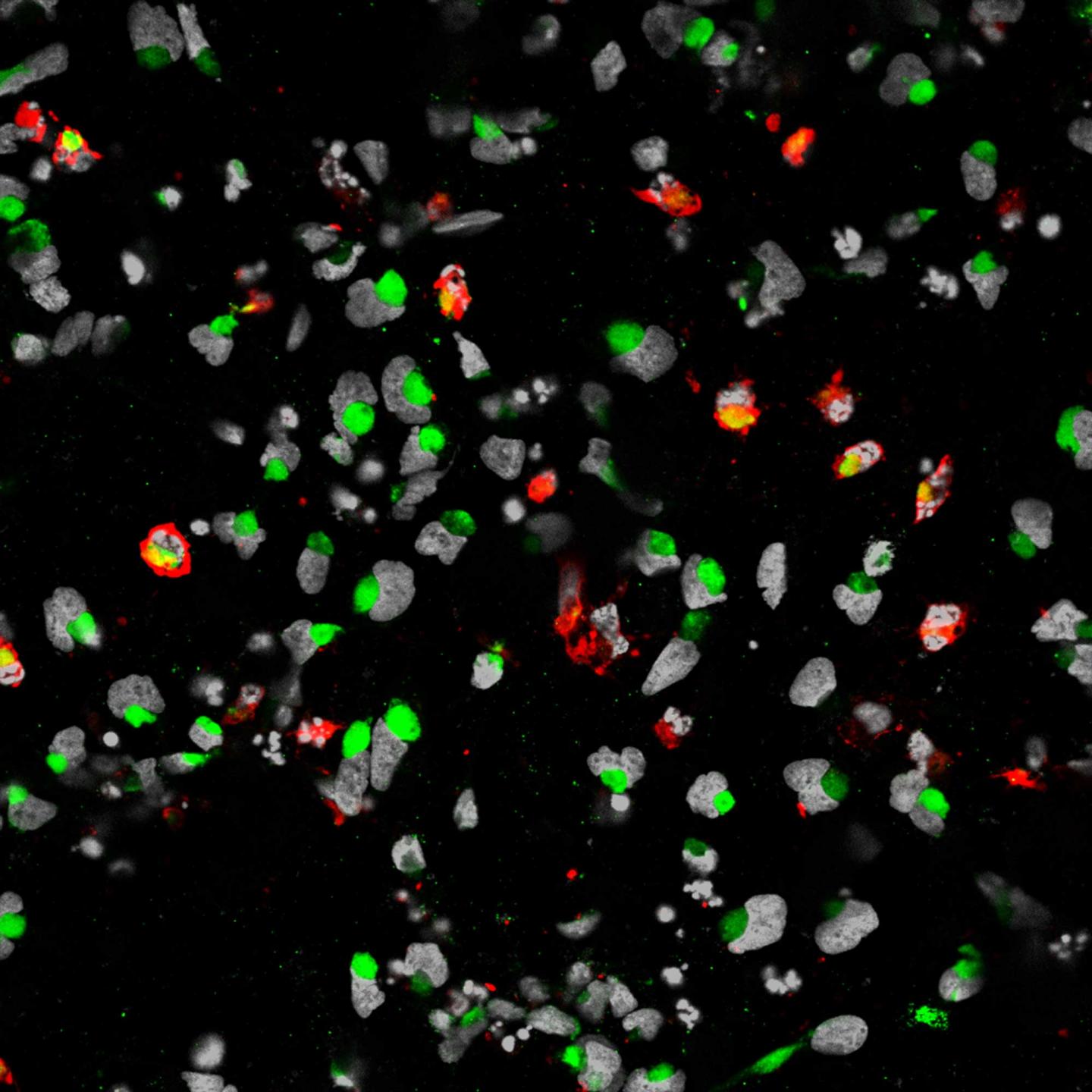 Credit: Sarah C. Ogden
|
|
Researchers Complete First Genome Analysis of the Zika Virus Outbreak An international team of researchers, led by scientists from the University of Oxford and the Evandro Chagas Institute in Brazil, have completed the first genome analysis of the Zika virus outbreak in Brazil. Their results, published March 24 in Science, provide new insights into how Zika reached the Americas and how the virus correlates with microcephaly. By sequencing the genomes of seven Brazilian Zika virus samples, the researchers demonstrated that Zika entered the Americas from a single introduction, which likely occurred between May and December 2013. During this timeframe, there was a 50% increase in the number of people traveling to Brazil via airplane from Zika-affected countries, such as Tahiti in French Polynesia. The researchers also reported that suspected microcephaly cases best correlated with Zika incidence around the 17th week of pregnancy, though they emphasized that correlation does not equal causation. “Our genome sequencing efforts have provided a clearer picture of the Zika virus in Brazil,” Dr. Márcio Nunes of the Evandro Chagas Institute said in a press release. “However, more genomic data are urgently needed to understand the origin, spatial spread and evolution of the virus in the Americas and in Brazil.” Which US Cities Are at Risk for a Zika Outbreak? Researchers from the National Center for Atmospheric Research (NCAR) have estimated the potential risk of a Zika virus outbreak for 50 cities within the United States, predicting that as temperatures rise this summer, cities as far north as New York City and as far west as Los Angeles could feel the impact of the virus. To pinpoint the geographical risk potentials, the researchers used two computer models simulating how a mosquito’s entire lifecycle is affected by meteorological conditions. They also weighed two other factors for each city: the number of incoming air travelers from Zika-affected countries and the percentage of households living below the poverty line. The map below shows the results of their analysis, published this March in PLOS Currents Outbreaks. “This research can help us anticipate the timing and location of possible Zika virus outbreaks in certain U.S. cities,” said NCAR scientist Andrew Monaghan, the lead author of the study, in a press release. “While there is much we still don’t know about the dynamics of Zika virus transmission, understanding where the Aedes aegypti mosquito can survive in the U.S. and how its abundance fluctuates seasonally may help guide mosquito control efforts and public health preparedness.” 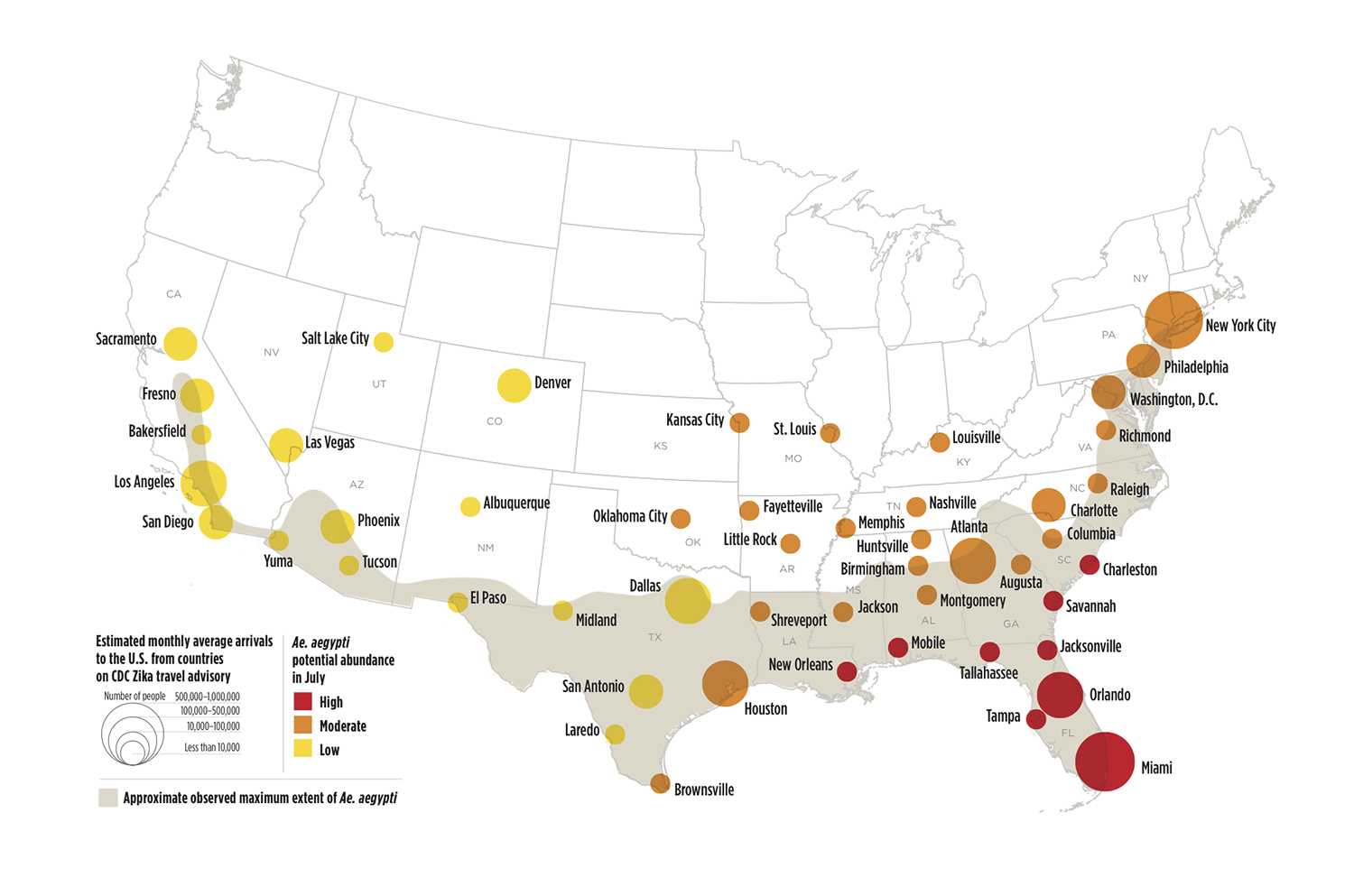 Credit: Image based on data mapped by Olga Wilhelmi, NCAR GIS program |