Antibiotic use promotes Clostridium difficile growth
Antibiotics have been effectively utilized for decades in the treatment against infectious agents. However, antibiotic use has been known to have detrimental effects, including the development of antibiotic resistant bacteria and alterations to the microbiota. The microbiota is a community of bacteria that colonize the body and can influence metabolism, physiology, nutrition, and immune function. An ever growing body of research indicates that the microbiota plays a critical role in regulating host homeostasis, and changes to the bacterial diversity of the microbiota may lead to increased susceptibility to disease.
Clostridium difficile is a bacterium that colonizes the intestine and can result in diarrhea and life-threatening colitis. C. difficile exists as spores that require specific bile acids to germinate and become growing bacteria. In the healthy intestine, C. difficile germination is prevented but infection is common after prolonged antibiotic treatment. The treatment for C. difficile infection is further antibiotic treatment, but antibiotic resistant strains have emerged. Researchers at North Carolina State University and The University of Michigan sought to understand how antibiotic use affects intestinal C. difficile growth.
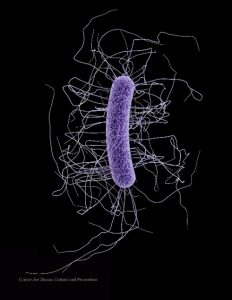
Source: CDC
The researchers examined the intestinal contents of mice before and after antibiotic treatment and found that C. difficile growth was supported in the small intestine regardless of antibiotic treatment but only supported in the large intestine following antibiotic treatment. Previous research has shown that bile acids are needed for C. difficile germination, so the researchers looked at concentrations of various primary and secondary bile acids before and after antibiotic treatment and found that secondary bile acid levels were depleted after antibiotic treatment. They then examined the effects of physiologically relevant levels of bile acids on C. difficile growth, revealing that primary bile acids, found in the small intestine, supported C. difficile growth, whereas secondary bile acids of the large intestine prevented C. difficile growth. Since the bacteria of the microbiota in the large intestine are responsible for the conversion of primary bile acids to secondary bile acids, the researchers then sought to identify which bacteria of the microbiota are important for secondary bile acid production. They found a strong correlation between the presence of the Lachnospiraceae and Ruminococcaceae family of bacteria and secondary bile acid concentration and C. difficile growth, indicating that these members of the microbiota may be critical in preventing C. difficile growth.
It is estimated that up to 50% of prescriptions for antibiotics are unnecessary or prescribed for inappropriate doses and duration. As antibiotics continue to be widely prescribed, strategies to prevent collateral damage from their use will be important to prevent the onset of additional diseases. In the case of C. difficile, strains of this bacteria are becoming increasingly resistant to antibiotic treatments, and future therapies may need to focus on bolstering secondary bile acid levels to inhibit C. difficile growth.
Anti-microbial compounds


