Researchers Generate ‘Living Medicine’ to Treat Drug-Resistant Infections
Scientists at the Centre for Genomic Regulation (CRG) and Pulmobiotics S.L have generated the first ‘living medicine’ to treat antibiotic-resistant bacteria growing on the surfaces of medical implants. The study published in the journal Molecular Systems Biology highlights a treatment that removes a common bacteria’s ability to cause disease and alternatively repurposes it to attack destructive microbes instead.
The new treatment aims to target biofilms, or colonies of bacterial cells that stick together on a surface, such as medical implants. Biofilm bacteria can be a thousand times more resistant to antibiotics than free-flowing bacteria. Medical implants happen to be an ideal growing habitat for biofilms, as they prevent antibiotics or the human immune system from destructing bacteria within the structure. The team of researchers hypothesized that involving living organisms to directly produce enzymes near biofilms is a safer and cheaper way to treat infections.
Engineering a Genome‐Reduced Bacterium to Eliminate Biofilms
Staphylococcus aureus is one of the most common species of biofilm-associated bacteria. This species does not respond to essential antibiotics, so patients must surgically remove any infected implants. Other options include the use of antibodies or enzymes, but such treatment methods are highly toxic to tissues and cells, causing adverse side effects.
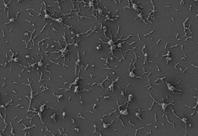
The researchers chose to engineer Mycoplasma pneumoniae, a common bacterium lacking a cell wall, to release therapeutic molecules to fight infections. M. pneumoniae also possesses a low risk of mutating and is unable to transfer modified genes to other nearby microbes.
The bacteria were initially modified to not cause illness, while additional engineering produced two different enzymes that dissolve biofilms and attack the cell wall of the bacteria. Further, the researchers modified the bacteria to expel antimicrobial enzymes.
First Steps to New Treatments for Medical Implant Infections
The engineered bacteria were tested on infected catheters in vitro, ex vivo and in vivo and successfully treated infections across all three experimental methods. Results show injecting therapy under the skin of mice treats 82% of infections among the animals.
ICEA Research Professor Luis Serrano, Director of the CRG and co-author of the study, notes the modified bacteria may also have long-term applications for other diseases. “Bacteria are ideal vehicles for ‘living medicine’ because they can carry any given therapeutic protein to treat the source of a disease,” he said. “One of the great benefits of the technology is that once they reach their destination, bacterial vectors offer continuous and localized production of the therapeutic molecule. Like any vehicle, our bacteria can be modified with different payloads that target different diseases, with potentially more applications in the future.”
These findings are a key first step for developing new treatments for infections impacting medical implants that are highly resistant to antibiotics. Catheters, pacemakers and prosthetic joints account for 80% of all infections acquired in hospital settings.
Related Research
Interested in drug resistance research? View more of our bacteria-related reagents here, or see more below:
- Cyclic Diguanosine Monophosphate from Stony Brook University
- Erythromycin A Production Plasmids from Tufts University
- Triclosan Resistant (mFabI) Cloning Plasmid from University of North Carolina Chapel Hill
- Bacillus subtilis ICDH Antibody from Tufts University
- LOBSTR E. coli Expression Strain from Massachusetts Institute of Technology


