Researchers Found a Way to Circumvent the Difficulty of Identifying Pancreatic Cancer
According to the Hirshberg Foundation for Pancreatic Cancer Research, pancreatic cancer has the highest mortality rate of all cancers. This is primarily due to most patients being diagnosed at a later stage. Patients in this category have a 5-year survival rate of 5%.
New findings from a study conducted by researchers at Queen Mary University suggest that a protein called Pentraxin 3 (PTX3) can be used as a biomarker for pancreatic ductal adenocarcinoma (PDAC). The study published in Precision Oncology quantifies the percentage of delayed diagnosis in 90% of patients with PDAC. The application of PTX3 as a biomarker for this cancerous pancreatic condition could decrease this statistic significantly.
The serum biomarker of interest (PTX3) showed a significantly higher sensitivity of 86% and specificity of 86% in comparison to the previously used CA19-9 with a wide sensitivity range from 41% – 86% and a specificity of 33% – 100%.
ELISA Kits and Monoclonal Antibodies Identify Increased Secretion of PTX3
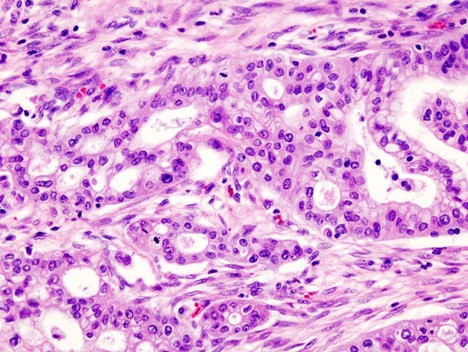
The study took on the form of a multi-center cohort where samples from patients with a pancreatic cancer diagnosis, patients with noncancerous pancreatic conditions and healthy volunteers were tested for PTX3 with ELISA kits. The Anti-PTX3 (MNB4) is a rat monoclonal antibody that was also used during the study and played a crucial role in the identification of PTX3 secretion predominantly surrounding the nucleus of pancreatic stellate cells (PSC).
PSCs lie in the exocrine regions of the pancreas and are noncancerous cells that surround the tumor. They exhibit high levels of PTX3 and hyaluronic acid secretion. Cancerous pancreatic cells on the other hand show minimal PTX3 secretion. The study determined that PSCs release PTX3 in response to signals from cancerous cells. Therefore, the level of PTX3 is indicative of the level of cancerous cells present.
The role of PTX3 expression in pancreatic cancer was investigated further by silencing the protein and observing its subsequent impact. The results indicated that hyaluronic acid deposition in the extracellular matrix stroma (ECM) and the invasion capacity of pancreatic stellate and cancer cells decreased when PTX3 expression was silenced.
What Does This Mean for Future Diagnosis and Treatment?
Professor of Liver and Pancreas surgery at Queen Mary University of London, Hemant Kocher, who led the study comments on previous methods of pancreatic cancer diagnosis. He emphasizes shortages of computerized tomography (CT) scanning saying that “CT scanning can detect the presence of a pancreatic mass, but it cannot distinguish pancreatic cancer from other non-cancerous pancreatic diseases.” Since the release of PTX3 is induced by signaling from cancerous cells to non-cancerous cells, PTX3 levels can bypass this shortcoming in CT scanning moving forward.
Not only will this study impact the methods of diagnosis in pancreatic cancer, but it may also modify the course of treatment moving forward. Researchers investigated the impact of chemotherapy targeting cancerous cells in the pancreas without targeting the ECM. This method had no effect on decreasing the level of PTX3 in the blood. Since the ECM stroma serves as a nutritional source for cancerous pancreatic cells, radiotherapy targeting the ECM caused PTX3 levels to decrease significantly.
Looking for more? Check out our collection of pancreatic and cancer cell lines below:
- KPCY Mouse Pancreatic Cancer Cell Lines from University of Pennsylvania
- Human Pancreatic Duct Epithelial Cell Line (H6c7) from University Health Network, Canada
- Human Ovarian Yolk Sac Tumor Cell Line NOY1 from Nagoya University
- Human Fibroblast Growth Fact 2 (FGF-2)-GST Protein from University of Buffalo
- SUMO2/SUMO3 [8A2] Antibody from The Johns Hopkins University
- L-MYC (CMV) Lentivirus


