Zika therapeutic targets identified using CRISPR technology
University of Massachusetts Medical School researchers, led by Kerafast providing investigator Dr. Abraham L. Brass, have used CRISPR technology to identify human proteins required for Zika virus infection and replication. These proteins now represent potential targets for the development of Zika treatments.
|
Zika is a flavivirus, a family of mosquito-trasmitted viruses that also includes dengue, West Nile and yellow fever. The recent Zika outbreak, which began in Brazil last year, has been linked to microcephaly in newborns, as well as Guillain–Barré syndrome (a disorder in which the immune system attacks the nerves) in adults. The virus has spread rapidly through South and Central America, and it has been declared a public health emergency by the World Health Organization. With no current treatments, cures or vaccines, the Zika virus has become an important and busy area of research.
The Brass lab has focused on the pathogenesis of various viruses, including those in the flavivirus family. As part of this work, the lab has developed a powerful suite of tools – including CRISPR/Cas9 and RNAi screening technologies, viral evolution analyses and mouse models – to explore how viruses exploit human host cells to replicate. Their tools allow for the identification of viral dependency factors that can represent potential therapeutic targets. |
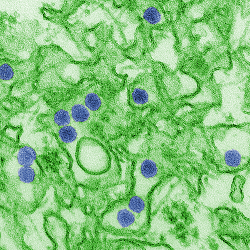 |
After the Zika outbreak, the Brass lab applied their CRISPR/Cas9 and RNAi screening technologies to discover potential Zika and dengue weaknesses. They began knocking out or depleting each individual protein in the human genome, one at a time, to see the subsequent effect on Zika or dengue replication in the absence of that protein. As a result, the team identified several human proteins critical to both Zika and dengue viral replication, including the AXL protein, used by the virus to enter cells, and the endoplasmic reticulum membrane protein complex (EMC), which is involved in transmembrane protein processing and maturation. These results were recently published in the journal Cell Reports.
“We plugged Zika virus into our system and immediately began studying it,” said Dr. Brass in a press release. “What might have taken much longer to build from the ground up, we were able to turn around in a few short months. Our goal was to get the screens done, find what the viruses need to grow, and then get the data out to the rest of the research community right away.”
With this information now available, the hope is that researchers can develop therapies that inhibit Zika and dengue by targeting these proteins. The approach of disrupting a virus’ ability to use a human host cell’s resources has worked successfully with other viruses, such as HIV and hepatitis C. The first step is identifying which of the 20,000+ human proteins to target, and this new study helps point the scientific community in the right direction for Zika and dengue.
“These viral dependencies on human proteins represent weaknesses that could potentially be used to prevent or stop infection,” Dr. Brass explained. “Just like any enemy, the more we know about how these viruses function and replicate, the better.”
The new study is not the Brass lab’s only recent publication on the Zika virus. In another paper in Cell Reports, the group demonstrated that the human protein IFITM3 can block Zika virus replication and prevent cell death. Found in almost every human cell, IFITM3 works to alter the cell membrane in a way that makes it more difficult for viruses to penetrate it. These results suggest that boosting the activity of IFITM3 may be a potential lead for developing a therapy that can inhibit Zika virus infection.
For more on recent Zika virus research, check out our previous blog post “New Findings on the Zika Virus”. And if you’re studying Zika in the lab, see if these available reagents could help your research:
- Double-stranded (dsRNA) antibody from Dr. Brass
- Zika virus antibody from Dr. James E. Crowe, Jr. at Vanderbilt University